The Empty Chair: Uncovering the Cost of Patient No-Shows

It’s a busy day at the clinic. The staff is ready, the rooms are prepped, and the schedule is packed. But as the clock ticks on, several patients fail to show up. The result? Wasted time, unused resources, and missed opportunities to provide care. For healthcare providers, this isn’t just an occasional inconvenience—it’s a persistent and costly problem that demands a solution.
Patient no-shows are not just a scheduling inconvenience—they represent a critical challenge for healthcare providers.
Understanding the Problem
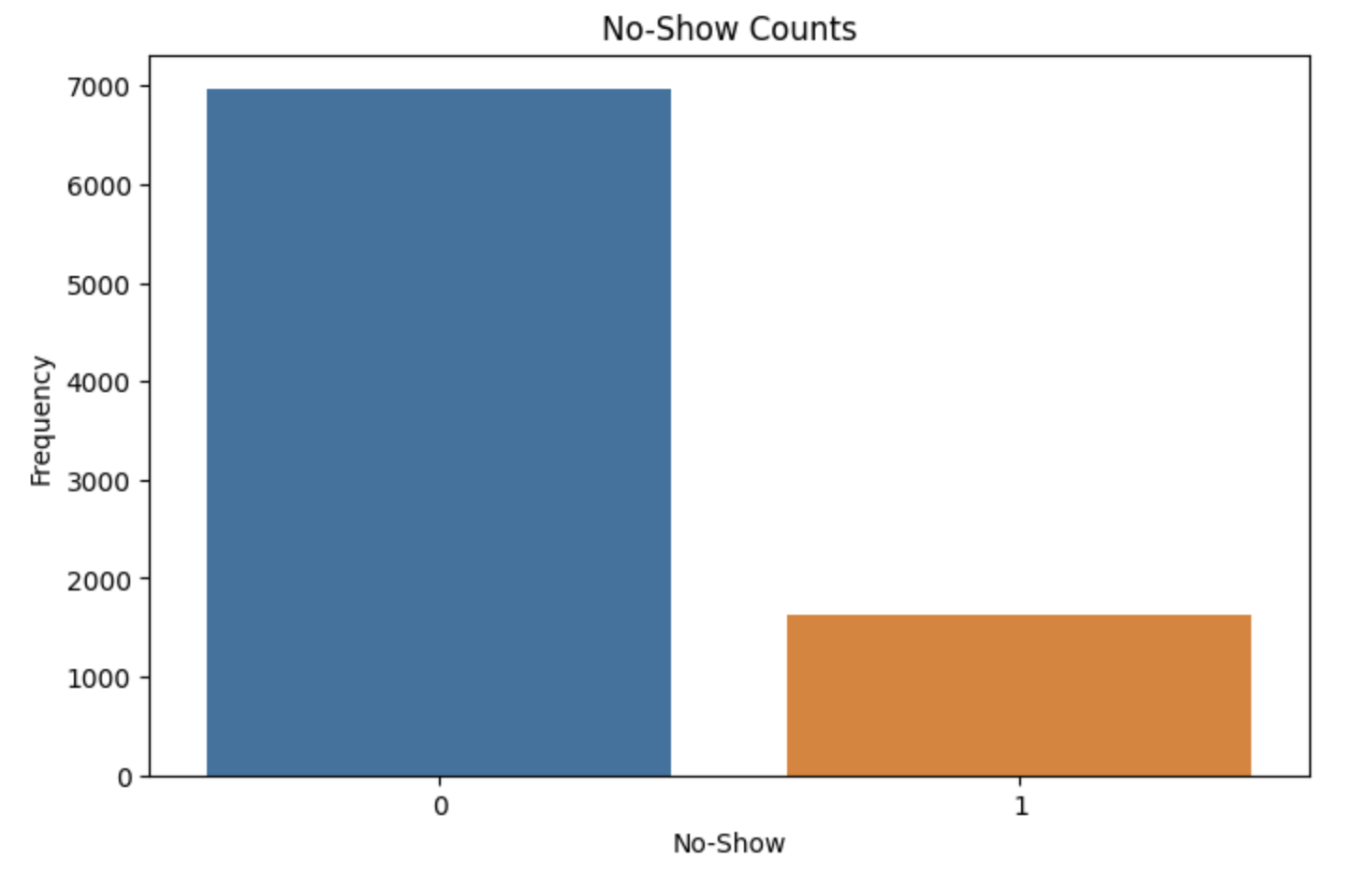
Patient no-shows occur when individuals fail to attend scheduled appointments without prior notice. While the reasons for missing an appointment vary—from forgetfulness to transportation issues—the consequences are universally negative for clinics and patients alike.
- Revenue Loss: Every missed appointment represents a missed opportunity for revenue. For smaller clinics, these losses can quickly add up.
- Wasted Resources: Clinics often allocate staff, rooms, and equipment for every scheduled appointment. No-shows mean wasted time and resources.
- Reduced Access: A no-show means that another patient, who could have used the slot, was unable to receive care.
- Long-Term Implications: High no-show rates can disrupt clinic efficiency and even lead to burnout among healthcare staff.
What Is A/B Testing?
Think of A/B testing as a controlled experiment where you compare two groups—Group A and Group B. The goal? To find out which approach leads to better outcomes. In the context of patient no-shows, I asked a simple question:
Does the type of appointment reminder affect whether a patient shows up?
- Group A: Patients received reminder emails.
- Group B: Patients received reminder phone calls.
- Group C: Patients received SMS reminders.
By tracking the no-show rates for each group, I could identify which reminder method was the most effective.
Why This Matters
A/B testing offers more than just a way to reduce no-shows—it empowers healthcare providers to:
- Make Data-Driven Decisions: Instead of guessing what works, clinics can rely on evidence.
- Personalize Patient Care: Insights from A/B tests can help tailor strategies to specific patient populations.
- Optimize Operations: Reducing no-shows improves clinic efficiency and ensures resources are used effectively.
A Sneak Peek at the Series
In the next post, we’ll dive deeper into how we designed this A/B test, from crafting the hypothesis to dividing patients into groups. You’ll learn about the importance of clean data, how to avoid biases, and the steps we took to ensure reliable results.